|
Case Report
Incidental rectal tonsil found on routine colonoscopy: A case report
1 DO, Department of Internal Medicine, Cooper University Hospital, Camden, NJ, USA
2 MD, Division of Gastroenterology, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA
Address correspondence to:
Sharmila Bisaria
Department of Internal Medicine, Cooper University Hospital, Camden, New Jersey,
USA
Message to Corresponding Author
Article ID: 100013G01SB2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Bisaria S, Patel D, Morgenstern R. Incidental rectal tonsil found on routine colonoscopy: A case report. Edorium J Gastroenterol 2021;8:100013G01SB2021.ABSTRACT
Introduction: Rectal tonsils, or benign lymphoid polyps are hyper-proliferative lymphoid tissue found in the intestine in the submucosa and lamina propria. Tonsils are follicles with germinal centers and surrounding mantle zone. Rectal tonsils are found incidentally on colonoscopy in the middle-aged due to age for routine colonoscopies. Rectal tonsils are mistaken for lymphoma and carcinoid tumors due to similar appearances. Identification through immunohistochemical workup prevents unnecessary workup for the concerning etiologies.
Case Report: A healthy 56-year-old female presented for a screening colonoscopy. A 9 mm sessile polyp was found in the rectum and removed. Pathology diagnosed rectal tonsil.
Conclusion: Due to similarity in appearance, they are mistaken for carcinoid tumors or lymphoma. They are distinguished from malignancy through immunohistochemical workup. It is imperative that rectal tonsils be removed for proper immunohistochemical staining to avoid unnecessary diagnostic and therapeutic workup for malignancy. There is no treatment for rectal tonsils. Due to concern for malignancy, they are removed, and so there is no discussion regarding outcomes of not removing a tonsil, or surveillance.
Keywords: Rectal polypoid lesions, Rectal polyp, Rectal tonsil
INTRODUCTION
Rectal tonsils, also known as benign lymphoid polyps are areas of hyper-proliferative lymphoid tissue found in the superficial layers of the intestine in the submucosa and lamina propria [1]. Tonsils are characterized by follicles with formed germinal centers with a narrowing surrounding mantle zone [1]. The number of hyperactive lymphoid complexes found throughout the tract increases from the right colon to the left, and commonly found in the rectum above the dentate line [2]. These complexes are larger in children and adolescents and become polypoid as they enlarge [2]. Rectal tonsils are found incidentally on routine colonoscopy. They have been found through evaluation of symptoms involving rectal bleeding or abdominal pain. Rectal tonsils often present in the middle-aged population due to age criteria for routine colonoscopies [3]. Rectal tonsils are mistaken for lymphoma and carcinoid tumors due to similarity in appearance. Proper identification through immunehistochemical workup prevents unnecessary workup for the concerning polyp etiologies. We will discuss a case of a rectal polyp found incidentally on routine colonoscopy screening and the workup involved afterwards.
CASE REPORT
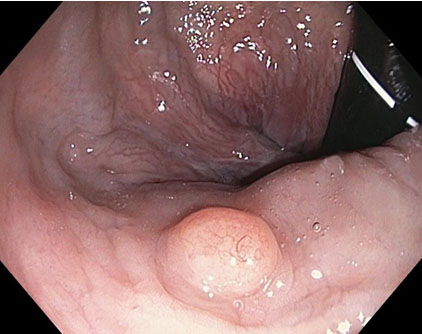
This case presents a 56-year-old Caucasian female with no medical history who presented for an elective routine colorectal cancer screening colonoscopy. She had no known family history of colon cancer or polyps. She was healthy and denied any gastrointestinal symptoms. The patient was noted to have a normal rectal exam. For the procedure, the colonoscope was passed through the anus under direct visualization and was advanced with ease to the cecum with retroflexion performed in the rectum. The quality of the preparation was noted to be good. Findings included small non-bleeding internal hemorrhoids. A single sessile polyp measuring 9 mm in size was found in the posterior wall of the rectum and was removed by cold snare polypectomy (Figure 1 and Figure 2). Another flat polyp measuring 6 mm in size was found in the splenic flexure and was completely removed by cold snare polypectomy.
On tissue pathology the polyp found in the rectum had a final diagnosis of polypoid colonic mucosa with nodular lymphoid hyperplasia, also known as a rectal tonsil. The specimen was found to have an underlying organized lymphoid nodule containing reactive germinal centers and surrounding mantle zone. Immunohistochemical stains showed a Bcl-2 negative reactive germinal center with intact CD20, CD21, and CD23 follicular dendritic cell meshwork. Kappa and Lambda immune-stains showed polytypic plasma cells with greater number of kappa positive cells, in part due to artificially stronger kappa staining. These findings confirmed reactive lymphoid proliferation and excluded lymphomas and non-neoplastic lymphoid proliferations such as lymphoid follicular proctitis.
The second polyp on pathology found at the splenic flexure was diagnosed as colonic mucosa with features consistent with sessile serrated adenoma without evidence of high-grade dysplasia. The patient was recommended to have a repeat colonoscopy in five years. In post-procedure, the patient had no complaints and remained healthy.
DISCUSSION
Rectal tonsils are areas of localized hyper-reactive lymphoid tissue found in the lamina propria of the gastrointestinal tract [4]. When evaluating a rectal tonsil, it is important to include neoplastic lymphomas [mucosa-associated lymphoid tissue (MALT) lymphoma, marginal zone B-cell lymphoma, mantle cell lymphoma, and follicular lymphoma] and non-neoplastic disorder (lymphoid follicular proctitis) in the differential diagnosis.
There have been only a few cases of rectal tonsils reported up until 2020 to our best knowledge [4]. These cases have included age groups from 1 to 71 years old with majority found at a mean age of 49 years old.
Although etiology of rectal tonsils is unclear, one case report demonstrated possible correlation with Epstein–Barr virus [1], while another case review found nodular lymphoid hyperplasia in various parts of the gastrointestinal tract in patients with immunodeficiencies, such as common variable immunodeficiency, selective IgA deficiency, human immunodeficiency virus, Helicobacter pylori, and Giardia infection [5].
Rectal tonsils are concerning as they resemble carcinoid tumors and lymphoma. It is possible to distinguish rectal tonsils from carcinoid tumors based on appearance as carcinoid tumors more often appear as solitary lesions, yellow in color [4]. Rectal tonsils are not unique in color and have a variety of physical manifestations. Most rectal tonsils are submucosal lesions while others present as polypoid, sessile, or as a nodule or mass [4],[6]. However, appearances should never be the distinguishing factor alone.
Immunohistochemical staining is the most accurate test to distinguish rectal tonsils from malignancy. A rectal tonsil is unique to neoplastic lymphomas due to its expression of CD20, CD21, and CD23 markers along with the presence of polytypic plasma cells and absence of Bcl-2 staining in the follicle [7]. Rectal tonsils are noted to have narrow surrounding mantle and marginal zones [7]. These findings are not seen in follicular or MALT lymphoma. Follicular lymphoma has prominent Bcl-2, Bcl-6, and CD10 staining and light chain restrictions [7]. Mucosa-associated lymphoid tissue lymphoma has prominent marginal zones and lymphoepithelial lesions including monoclonality of CD43 and presence of immunoglobulin light chain restrictions [4]. Mucosa-associated lymphoid tissue lymphomas can also have small to medium lymphocytes with a moderate amount of clear cytoplasm, indented or round nuclei, and absent or small nucleoli [7]. We were able to exclude marginal zone B-cell lymphoma as this will show follicular colonization with neoplastic B cells that replace reactive follicles and will co-express CD43 marker. Marginal zone B-cell lymphoma will also show a monotypic light chain pattern with either kappa or lambda immune-stains rather than polytypic plasma cells as seen in a rectal tonsil [7]. Mantle cell lymphoma was excluded from the differential as this will show expansion of mantle zones and neoplastic B-cells replacing follicles with co-expression of CD5 and cyclin D1. Finally, follicular lymphoma was excluded as this will typically present as monotypic follicle centers of neoplastic B cells with co-expression of CD10, Bcl-6, and Bcl-2 [7]. Lymphoid follicular proctitis, a non-neoplastic disorder, is characterized by a diffuse hyperplasia of lymphoid follicles with a granular mucosa, whereas a rectal tonsil is a nodular lymphoid aggregate with follicles [2].
The majority of rectal tonsils are asymptomatic such as in our case. Symptoms reported in previous cases include abdominal pain or rectal bleeding, which led to a colonoscopy and finding of a rectal tonsil [3]. It is unclear if the rectal tonsil was the cause of these symptoms or if it was an incidental finding.
Endoscopic ultrasound (EUS) can also aid in the workup of a submucosal lesion, such as a rectal tonsil, when a submucosal lesion is suspected. On EUS, a rectal tonsil appears as a well-demarcated, homogenous hypoechoic solid lesion that is located in the submucosa layer and/or lamina propria [7]. However, a rectal tonsil often mimics a rectal polyp and therefore, EUS is not performed in all cases and a complete resection is required instead for histology.
There is no specific treatment or surveillance that has been discussed in previous case reports regarding rectal tonsils. Due to concern for malignancy, a rectal tonsil is completely removed for diagnosis. Therefore, there has been no discussion regarding harmful outcomes of not removing a rectal tonsil, or proper surveillance needed with repeat colonoscopy.
CONCLUSION
Rectal tonsils are found in the submucosa of the rectum on routine colonoscopy. Due to their resemblance with lymphoma and carcinoid tumor, they raise concern when found on colonoscopy. It is imperative that diagnosis of a rectal tonsil is made with complete resection of the tonsil and immunohistochemical testing to distinguish it from malignancy and avoid excessive workup and treatment.
REFERENCE
1.
Kojima M, Lijima M, Shimizu K, Hoshi K. Localized lymphoid hyperplasia of the rectum representing progressive transformation of the germinal center. A report of two cases. APMIS 2007;115(12):1432–6. [CrossRef]
[Pubmed]

2.
Farris AB, Lauwers GY, Ferry JA, Zukerberg LR. The rectal tonsil: A reactive lymphoid proliferation that may mimic lymphoma. Am J Surg Pathol 2008;32(7):1075–9. [CrossRef]
[Pubmed]

3.
Homan M, Volavšek M. Rectal tonsil. J Pediatr Gastroenterol Nutr 2012;54(5):575.
[Pubmed]

4.
Takehara M, Muguruma N, Kitamura S, et al. Twin rectal tonsils mimicking carcinoid or mucosaassociaited lymphoid tissue lymphoma. Clin Endosc 2017;50(5):500–3. [CrossRef]
[Pubmed]

5.
Albuquerque A. Nodular lymphoid hyperplasia in the gastrointestinal tract in adult patients: A review. World J Gastrointest Endosc 2014;6(11):534–40. [CrossRef]
[Pubmed]

6.
Alshamali Y, Taleb A, Al-Taweel T. Rare benign large lymphoid colonic polyp. Case Rep Gastrointest Med 2018;2018:5758689. [CrossRef]
[Pubmed]

7.
Hong JB, Kim HW, Kang DH, et al. Rectal tonsil: A case report and literature review. World J Gastroenterol 2015;21(8):2563–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
We would like to thank Hahnemann University Hospital for providing us with the opportunity to discover this case.
Author ContributionsSharmila Bisaria - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dhruvan Patel - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ricardo Morgenstern - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Sharmila Bisaria et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.