|
Case Report
Chylothorax: A rare complication of severe necrotizing pancreatitis
1 Department of Gastroenterology & Hepatology, University of Connecticut Health Center, Farmington, CT, USA
2 Department of Medicine, University of Connecticut Health Center, Farmington, CT, USA
Address correspondence to:
Murali Dharan
MD, 263 Farmington Avenue, Farmington, CT 06030,
USA
Message to Corresponding Author
Article ID: 100017G01MM2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Mavilia MG, Grover D, Dharan M. Chylothorax: A rare complication of severe necrotizing pancreatitis. Edorium J Gastroenterol 2021;8:100017G01MM2021.ABSTRACT
Introduction: Chylothorax is a rare complication of pancreatitis with only two case reports of chylothorax secondary to acute pancreatitis in the current literature.
Case Report: A 49-year-old female presented with dyspnea and fatigue approximately three months after an episode of complicated acute necrotizing pancreatitis. She was found to have a large right-sided chylothorax.
Conclusion: Due to the intimate relationship between the pancreas and lymphatic drainage system, it is likely that her extensive pancreatic inflammation caused obstruction and/or direct injury to her thoracic duct, leading to development of chylothorax.
Keywords: Chylothorax, Pancreatic necrosis, Pancreatitis, Thoracic duct injury
INTRODUCTION
Chylothorax is a rare cause of pleural effusion with lymph fluid accumulation in the pleural space [1] characterized by milky pleural fluid with high triglyceride levels (>110 mg/dL) [2]. The etiology can be traumatic (50%), nontraumatic (44%), or idiopathic (6%) [3]. Chylothorax is most often seen after mechanical injury to the thoracic duct (TD) by trauma, surgery, or malignancy. Atraumatic etiology includes infection, lymphoma, congenital defects, lymphangioleiomyomatosis, superior vena cava (SVC) thrombosis, sarcoidosis, amyloidosis, and cirrhosis [1]. Rarely chylothorax can be a complication of pancreatitis. There is scant literature [4],[5],[6],[7],[8],[9],[10],[11],[12],[13] about chylothorax caused by pancreatitis with only two case reports of chylothorax secondary to acute pancreatitis [4],[5]. We present a case of severe necrotizing pancreatitis complicated by large chylothorax.
CASE REPORT
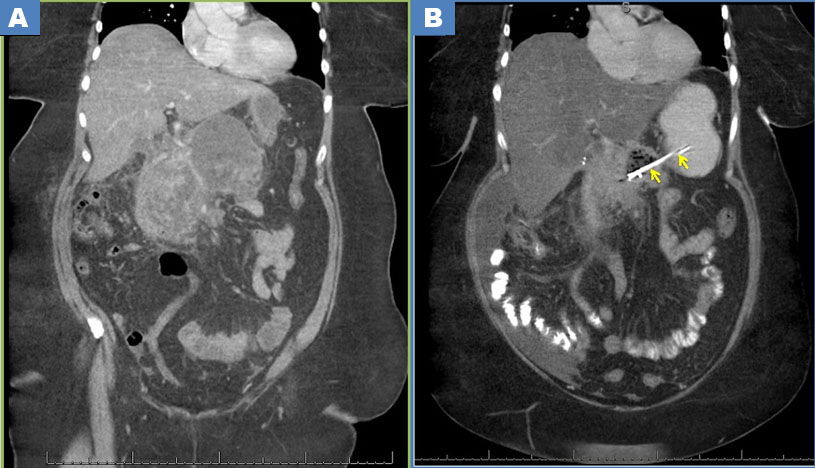
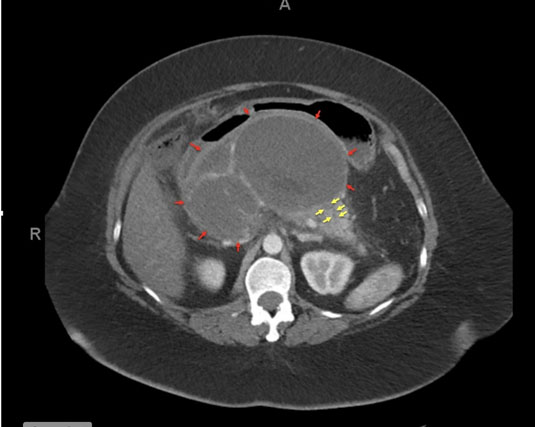
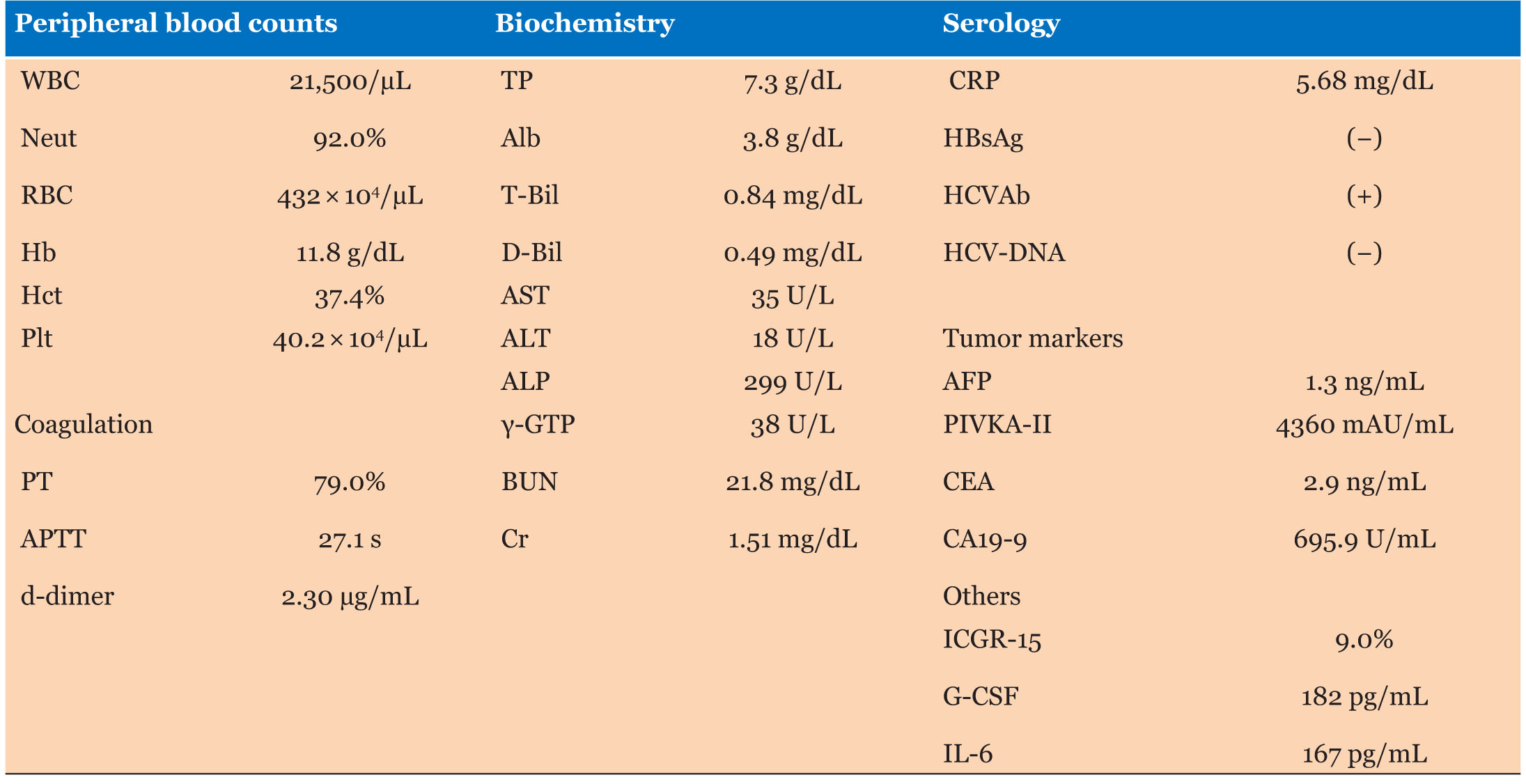
A 49-year-old obese female was admitted with acute necrotizing pancreatitis secondary to gallstone disease and heavy alcohol use (21–28 drinks/week). After conservative management she underwent cholecystectomy. Two weeks later she was admitted with abdominal pain and anorexia. Evolving large multiloculated peri-pancreatic collections with mass effect on the stomach and liver (Figure 1A) and portal/superior mesenteric vein thrombosis were noted on imaging and she was started on apixaban (Eliquis). Six weeks after the pancreatitis, endoscopic ultrasound (EUS) cystogastrostomy drainage of pseudocyst/walled-off peri-pancreatic necrosis (WOPN) was performed for persistent symptoms. The peri-pancreatic collection shrunk (Figure 1B) and symptoms improved following necrosectomy and washout. Two double pigtail plastic stents were placed through the cyst-gastrostomy to manage disconnected pancreatic duct which was identified radiologically (Figure 2). Three weeks later (three months after her initial episode) she presented with progressive dyspnea and fatigue. No recent travel, trauma, or personal/family history of malignancy was reported. The patient was afebrile, tachycardic with stable hemodynamics and required oxygen supplementation. Breath sounds at the right lung base were diminished. Complete blood count (CBC) and serum chemistry were unremarkable with sodium of 139 mmol/L, potassium of 3.8 mmol/L, chloride 104 mm/L, blood urea nitrogen of 7 mg/dL, creatinine 0.6 mg/dL, non-fasting glucose of 119 mg/dL, aspartate aminotransferase (AST) 24 U/L, alanine aminotransferase (ALT) 12 U/L, alkaline phosphatase 97 U/L, total bilirubin 0.7 mg/dL, and total protein of 6.4 g/dL. Chest X-ray revealed a large right-sided pleural effusion (Figure 3). Transthoracic echocardiogram showed preserved left ventricular ejection fraction without diastolic dysfunction. A chest tube was placed, draining 1000 cc of milky fluid. Pleural fluid analysis showed protein 2.3 g/dL, lactate dehydrogenase (LDH) 141 U/L, glucose 123 mg/dL, amylase 18 U/L (normal), and triglycerides 133 mg/dL (elevated). On fluid cytometry reactive mesothelial cells without evidence for malignancy were noted. Routine cultures were negative. Findings were consistent with a chylothorax. She was started on a low-fat diet. Thoracostomy tube remained in place for seven days and was removed when output reduced and her symptoms improved. The patient was discharged with a close follow-up and continued dietary modification. There was consideration for future use of octreotide in the event that chylothorax were to recur or become uncontrolled with dietary modification alone.
DISCUSSION
Chylothorax is an uncommon cause of pleural effusion with an incidence of 1 in 6000 patients. It is more common in females (male:female ratio of 1:21) and in older individuals (median age: 64 years) [14]. It usually presents as unilateral right-sided pleural effusion, however, laterality depends on anatomy of TD disruption. Disruption above the level of T5 vertebrae causes a left-sided effusion, whereas damage below T5 results in a right-sided effusion [6].
Several possible mechanisms may contribute to development of a chylothorax and the predominant pathway may be different for acute interstitial, acute necrotizing, and chronic pancreatitis. Inflammation and fluid collections related to pancreatitis may compress/obstruct the TD. Inflammation of lymphatic structures in the chest can impede flow of lymph via the thoracic duct causing chylous effusion [5]. In the setting of necrotizing pancreatitis, direct injury to of abdominal TD is possible. Pancreatitis can cause chylous ascites due to disruption of the abdominal TD, with trans-diaphragmatic leakage into the pleural space [7]. Chylothorax in chronic pancreatitis is usually associated with chylous ascites [7],[8],[9],[10]. There is one case report of recurrent pancreatitis with fistulous erosion of pseudocyst causing pleural effusion that morphed into chylothorax after repeated thoracentesis [11].
Conversely, acute pancreatitis has also been reported after TD obstruction. It is possibly related to anatomy of lymphatic pathways and their proximity to the pancreas whose blockage can cause edema and inflammation of the pancreatic parenchyma [15],[16]. This anatomic relationship may explain lymph flow disruption after pancreatitis.
Chylothorax is typically detected shortly after the initial insult, particularly in post-surgical cases. Patients usually present with dyspnea, cough, ascites, anorexia, or weight loss. Normally, the body produces 1.5–4 L of chyle daily [1] and rapid accumulation in the pleural space can occur with TD disruption.
Our patient had a relatively late presentation of chylothorax, occurring three months after onset of pancreatitis. We hypothesize that this was in part due to increase in lymph return during her recovery from pancreatitis. In the first several weeks, she experienced significant nausea and anorexia. With improvement in abdominal symptoms and oral intake (including high fat diet) more lymph flow was likely diverted into her pleural space. Direct injury to TD from WOPN and subsequent fibrosis likely contributed to delayed chylothorax. In one previously reported case [2], chylothorax presented approximately two weeks after necrosectomy. A similar time course was seen in our patient. If chylothorax was caused by compression of the TD alone, we would have expected an earlier presentation and resolution of the pleural effusion following drainage of WOPN. The patient had insufficient ascites for paracentesis and it is unclear if she had chylous ascites and trans-diaphragmatic spread.
Given paucity of data, there are no definitive guidelines for treatment of chylothorax secondary to pancreatitis. Conservative management includes diet modification and drainage of the effusion [1]. Low fat diet can decrease chyle production and fluid accumulation. Octreotide has been used to reduce splanchnic blood flow and thereby decrease lymph flow, but efficacy data are limited [1]. Further management depends on the etiology and the volume and rate of fluid accumulation. Higher daily chest tube output requires intervention with pleurodesis, TD ligation and/or surgical repair. Pleurodesis without TD repair had a success rate of 80–100% in one case series [1]. In a retrospective analysis [3], 77% of the patients were initially managed conservatively, but surgical intervention was required in 59%. This study also noted more frequent reaccumulation in non-traumatic chylothorax.
CONCLUSION
Albeit rare, chylothorax is an important complication of acute pancreatitis that should be recognized. This can occur due to injury to the thoracic duct in the setting of extensive pancreatic inflammation and necrosis. When endoscopic intervention including necrosectomy is warranted, chylothorax and attendant respiratory implications add complexity to procedural sedation.
REFERENCE
1.
Bender B, Murthy V, Chamberlain RS. The changing management of chylothorax in the modern era. Eur J Cardiothorac Surg 2016;49(1):18–24. [CrossRef]
[Pubmed]

2.
Staats BA, Ellefson RD, Budahn LL, Dines DE, Prakash UB, Offord K. The lipoprotein profile of chylous and nonchylous pleural effusion. Mayo Clin Proc 1980;55(11):700–4.
[Pubmed]

3.
Ryu JH, Tomassetti S, Maldonado F. Update on uncommon pleural effusions. Respirology 2011:16(2);238–43. [CrossRef]
[Pubmed]

4.
Teoh JYC, Teoh AY, Chiu PWB, Ng EK. Chylothorax as a rare complication after severe necrotizing pancreatitis and endoscopic pancreatic necrosectomy. Gastrointest Endosc 2013;77(3):498–500. [CrossRef]
[Pubmed]

5.
6.
7.
Goldfarb JP. Chylous effusions secondary to pancreatitis: Case report and review of the literature. Am J Gastroenterol 1984;79(2):133–5.
[Pubmed]

8.
Blanchon P, Hivet M, Naudin G, et al. Chronic pancreatitis and chylous ascites. Discussion of a case. [Article in French]. Ann Med Interne (Paris) 1972;123(5):491–5.
[Pubmed]

9.
Fourdan O, Lévy P, Sauvanet A Bernades P. A case of chylous ascites associated with exudative enteropathy complicating chronic pancreatitis of alcoholic origin. [Article in French]. Gastroenterol Clin Biol 1993;17(1):53–5.
[Pubmed]

10.
Collery P, Coudoux, Geoffroy H. Chylous ascites and chronic pancreatitis. [Article in French]. Med Chir Dig 1978;7(1):9–13.
[Pubmed]

11.
Kiss J, Gödry G. Chylothorax as a rare complication of pancreatitis. [Article in Hu]. Magy Seb 2000;53(5):220–2.
[Pubmed]

12.
13.
McGrath EE, Blades Z, Anderson PB. Chylothorax: Aetiology, diagnosis and therapeutic options. Respir Med 2010;104(1):1–8. [CrossRef]
[Pubmed]

14.
García J, Alemán C, Jáuregui A, Vázquez A, Persiva Ó, Fernández de Sevilla T. Chylothorax in adults. Characteristics of 17 patients and a review of the literature. Arch Bronconeumol 2017;53(7):407–8. [CrossRef]
[Pubmed]

15.
Michel P, Pagliano G. Acute chyloperitoneum. [Article in French]. J Chir (Paris) 1992;129(12):544–9.
[Pubmed]

16.
Bedat B, Scarpa CR, Sadowski SM, Triponez F, Karenovics W. Acute pancreatitis after thoracic duct ligation for iatrogenic chylothorax. A case report. BMC Surg 2017;17(1):9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Marianna G Mavilia - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dheera Grover - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Murali Dharan - Conception of the work, Design of the work, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Marianna G Mavilia et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.